How is this condition diagnosed?
On initial assessment at Momentum Spine & Sport Physiotherapy your physiotherapist will perform an examination that will start with your child’s history. They will ask questions about when your child’s pain began, when and where precisely the pain occurs, your child’s activity levels, whether there have been any previous spinal injuries, whether there are any problems with urination or bowel movements, whether there are any muscle weaknesses, and what makes your child’s pain better or worse. They will also want to know if your child complains of pain in any other areas of their body such as their hips or knees. They may also ask questions about school and sport activities, activities at home, your child’s moods, and whether or not they have had a fever associated with their pain.
A physical examination will be done once the history is complete. Your physiotherapist will examine your child’s back to evaluate the curves of the spine, spasm of the muscles, overall posturing and alignment of the back and lower extremities, and for unusual markings on the skin or soft tissues along the spine. They will palpate, or touch along the spine and over the muscles to determine if any particular areas are painful or tight. They may push on the spine, or manually move the spine to get a general idea of how much motion is available at each segment.
Your physiotherapist will also examine your child’s hips, knees, and ankles to determine if these joints and the muscles that are involved with them might be contributing to the pain your child feels in their back. The length (flexibility) and strength of the muscles of the buttocks, the front of the hip, as well as the thigh (quadriceps and hamstrings muscles) are particularly important areas that your therapist will assess. These muscles can pull on the back if they are too tight, or not support the back well enough if they are too weak. Both tightness and/or weakness can lead to back pain. The hip joints themselves, if restricted in motion, can lead to back pain so their motion will be thoroughly assessed. The hips are designed to be mobile enough so that your trunk can turn and move freely especially when twisting or extending the spine. If the hip joints become restricted or tight there is less motion available in the joint. The decreased motion found in the hips is then often made up for by increased movement occurring in the back instead, which can lead to pain.
Your physiotherapist will also want to examine your child’s ability to bend their back forwards, backwards, sideways, as well as rotate it and to get into positions involving a combination of these motions. Your physiotherapist will also look at your child’s posture and alignment while they are standing and sitting, and may also want to watch your child during different activities such as walking, squatting, jumping, lifting one leg, or kneeling on their hands and knees. The ability for your child’s trunk to be supported by the deep muscles of the abdominal area and back will be determined by your therapist as they observe your child performing these activities.
A neurological examination may need to be done which will include checking your child’s reflexes, sensation, and muscle strength.
Imaging studies
X-rays are recommended for most children complaining of back pain due to the fragile nature of their developing spine. Views of the spine from the front, the side, and part way in between (oblique) should be taken. X-rays will allow examination of bone as well as the disc spaces.

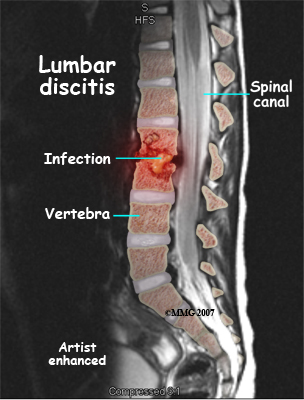
An MRI may be required if further examination of the spine is needed. An MRI machine uses magnetic waves, not X-rays, to show the soft tissues of the body. These tissues include the spinal cord, nerves, and discs. It can also evaluate spinal bones. An MRI allows your healthcare professional to look at slices of the area in question. The test may require the use of dye in an IV. Sedation or anesthesia may be needed to help your child lie still for this test.
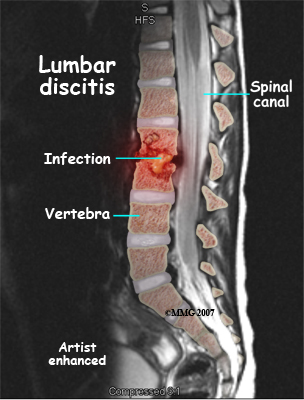
A computed tomography (CT) scan may also be ordered. This test is best for evaluating problems with the vertebral bones. Children usually tolerate this test well, however, this test exposes them to radiation, which is significantly higher than during plain x-rays. Sometimes this test may require dye in the spinal canal fluid for easier identification of the spinal cord and nerve root anatomy. When dye is injected for this purpose, the technique is called a myelogram.
Bone scans, also called nuclear scans, can be used to detect fractures, bone infections, or tumors. A radioactive tracer, Technetium, is injected into your child’s vein and any area where there is an increase in metabolic activity the Technetium will show up as being more concentrated. Increased metabolic activity occurs when there is inflammation, a fracture, an infection, or a tumor. Some tumors in the spine can spread to other parts of the body, or come from cancer somewhere else in the body. A scan can be helpful to see if there are other areas in the body where the cancer may be.
SPECT imaging is often added after a bone scan to provide information that is not available on routine bone scan images. SPECT stands for Single Photon Emission Computed Tomography. It provides three-dimensional (3-D) views of the area examined. Following a bone scan your child will remain on the exam table and the camera will rotate around the table while it takes pictures. SPECT imaging adds 30 to 60 minutes to the time of the nuclear scan. Sedation may be needed.
A biopsy of the spine may be required if an infection or tumor is found. In some cases tissue samples can be taken with a needle but in other cases a minor surgery is needed to obtain the tissue biopsy as this allows the doctor a better view of the area he or she needs to biopsy. The tissue is then looked at under a microscope.
Laboratory Studies
Blood tests may be requested to evaluate the blood for specific bacteria causing an infection. A complete blood count (CBC), especially in children under the age of 10, is important as the chance that back pain is from leukemia is greater in children younger than 10. If there is an infection, the CBC may show an increase in the infection-fighting white blood cells. A C-reactive protein (C-RP) and erythrocyte sedimentation rate (ESR) may also show an increase when an infection is present. A blood culture may be necessary to help determine which bacteria are causing the infection in discitis or vertebral osteomyelitis.
In some cases a biopsy may be required to determine which bacteria is the culprit. Knowing which bacteria is present will help your doctor choose the right antibiotic to treat the infection.
Momentum Spine & Sport Physiotherapy provides services for physiotherapy in Edmonton and St Albert.

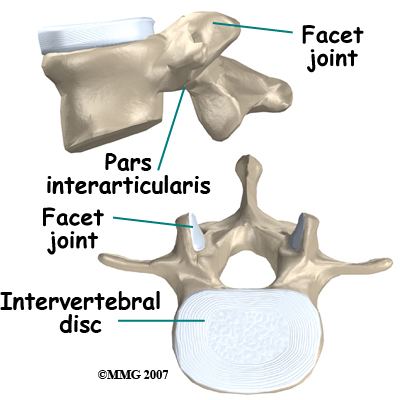 The spine is made up of a column of bones. A round block of bone, called a vertebral body, forms the biggest portion of each segment, or vertebrae. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord.
Facet joints are small joints on either side of the spine that allow motion. As the bones of the spine interlock, a facet joint is formed. Each vertebra will form two facet joints, on either side. There is a pair at the top and a pair at the bottom of each vertebra. The area of the vertebra that connects the large body of the vertebra to the facet joints is called the pars articularis or pedicle.
The part between the two sets of facet joints is the lamina.
The spine is made up of a column of bones. A round block of bone, called a vertebral body, forms the biggest portion of each segment, or vertebrae. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord.
Facet joints are small joints on either side of the spine that allow motion. As the bones of the spine interlock, a facet joint is formed. Each vertebra will form two facet joints, on either side. There is a pair at the top and a pair at the bottom of each vertebra. The area of the vertebra that connects the large body of the vertebra to the facet joints is called the pars articularis or pedicle.
The part between the two sets of facet joints is the lamina. 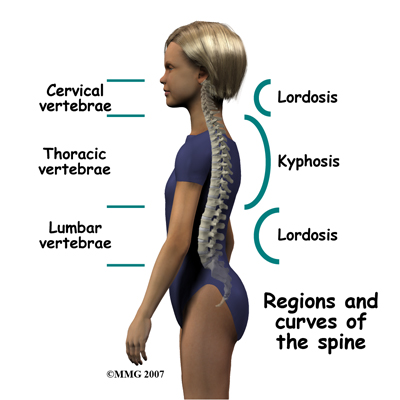


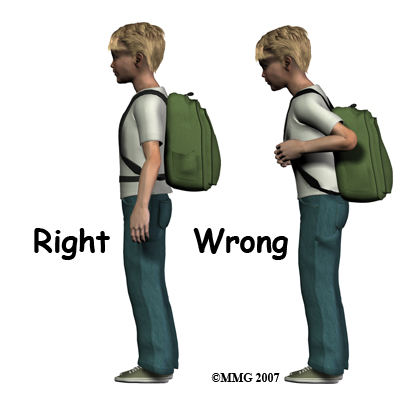 Carrying backpacks may sometimes be to blame for non-specific back pain. Your physiotherapist will discuss this with your child and may ask to see the backpack that your child regularly uses. Many children these days carry extremely heavy backpacks and use backpacks that are poorly designed ergonomically. It is suggested that children wear their backpack using both shoulder straps and that if there is a waist or chest strap, that these straps also be used. When purchasing a backpack, ensure the shoulder straps are wide, padded, and adjustable so that the weight can be evenly distributed. As a general rule backpacks should not be heavier than 10% of your child’s body weight. Making more frequent trips to the locker can decrease the weight of the backpack, and packing the backpack so the weight is distributed evenly can also decrease the strain on the back. Using a wheeled backpack may be an option and should be considered if your child suffers from frequent back pain, or is recovering from an injury.
Carrying backpacks may sometimes be to blame for non-specific back pain. Your physiotherapist will discuss this with your child and may ask to see the backpack that your child regularly uses. Many children these days carry extremely heavy backpacks and use backpacks that are poorly designed ergonomically. It is suggested that children wear their backpack using both shoulder straps and that if there is a waist or chest strap, that these straps also be used. When purchasing a backpack, ensure the shoulder straps are wide, padded, and adjustable so that the weight can be evenly distributed. As a general rule backpacks should not be heavier than 10% of your child’s body weight. Making more frequent trips to the locker can decrease the weight of the backpack, and packing the backpack so the weight is distributed evenly can also decrease the strain on the back. Using a wheeled backpack may be an option and should be considered if your child suffers from frequent back pain, or is recovering from an injury.
